N/A
“My wife has been bugging me to get this checked out for a while, what do you think?”
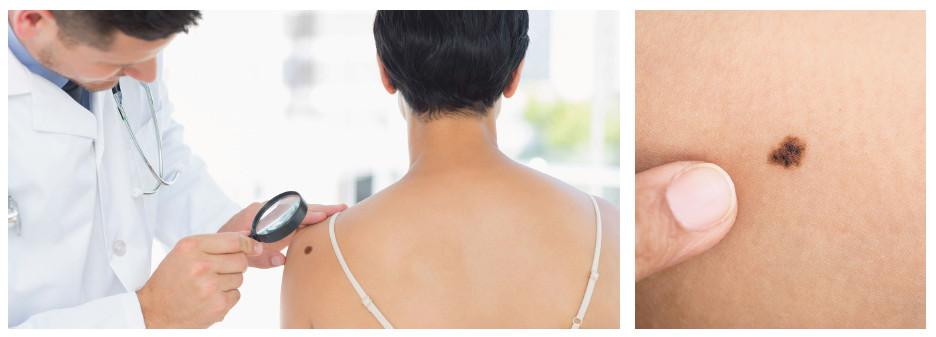
I lean forward and peer at the dark, ugly mole. It appears to be what we call a seborrheic keratosis, something completely harmless. But clinical experience tells me that it pays to be thorough, so I fetch my dermatoscope from my pocket.
My patient suddenly appears nervous. “What’s that, doctor?” he asks. “Will it hurt?”
“Not at all,” I reassure him. “This will just help me to distinguish if you have a good or a bad mole.”
“Is it like a biopsy?”
“No, but it’s almost as accurate as a biopsy in good hands,” I tell him. “This is just an augmentation lens with polarized light so that I can get a closer look. If your mole looks benign under the dermatoscope, then we don’t need to make a cut.”
“That’s great!” he says.
Dermoscopy
He’s certainly not the only patient I’ve had this conversation with. Skin tumors are probably the most common cancers in the world, and one of my most frequent tasks is to examine moles such as these. The skin is a very large organ, frequently exposed to the sun and to viral infections—and these two factors put together are chiefly responsible for the emergence of skin cancer. The danger is especially high in fair-skinned people of northern European origins who live and work in the subtropical zone (as do many Western expatriates in our community here) because their skin is not genetically prepared for solar radiation levels in these parts. For these people in particular, early diagnosis of melanoma is critical.
This is why dermoscopy is so important. A dermatoscope is a magnifying lens with a polarizing light. The way you position the lens and whether or not you use polarization reveals different tissue structures within the mole with great clarity. This simple instrument makes it much more straightforward to diagnose and distinguish melanomas that need to be removed from benign lesions, which do not need to be removed at all.
When I place the dermatoscope on the patient’s mole, I get a very different picture of the seemingly benign tumor. Through the lens, I see variations in color. I see irregular blue-white veil. I see a honeycomb-like structure at the edges. I see whitish areas of atrophy. All of this tells me that there is nothing benign about this mole after all. This patient is in fact harboring a malignant melanoma in his skin—a mass of cancerous tissue that will certainly kill him if he doesn’t have the whole tumor removed as soon as possible.
My point is this: you can’t always trust the naked eye when it comes to distinguishing a melanoma from a harmless mole. That’s a problem, because there are people out there with hundreds of moles all over their body, and you can’t simply dig them all out. I had another patient who was covered in moles, and there was melanoma history in her family, which meant that her risk was higher than normal. When I examined her, I did indeed find a lesion that I suspected to be a melanoma, which had to be removed. But there were also other lesions that may or may not have been cancerous; it was too hard to tell just by looking. To make things more complicated, this patient suffered from keloids—meaning that every surgical procedure would leave an ugly scar. If we removed too few, it might kill her eventually—she would die from a melanoma. But if we cut out too many, she would become a Frankenstein.
On the Safe Side
You’d think that a dermatologist would carry a dermatoscope like a cardiologist would a stethoscope, but in fact the whole field of dermoscopy isn’t widely practiced outside of Europe and Australia. I would say that probably half of American dermatologists wouldn’t use it regularly. This is a pity, because it’s an incredibly effective diagnostic method.
Dermoscopy has been known since the seventeenth century, but consistent research really got going around 40 years ago, with most activity based in Graz, Austria. It was conducted to increase the accuracy of skin cancer diagnosis by classifying structures in moles that are visible under a dermatoscope against biopsy findings from confirmed melanomas and other cancers. By slowly matching their data to the results of tissue examination, these researchers confirmed that dermoscopy could be used to accurately identify a melanoma. This is why we can trust this medical field, because it has been subjected to a rigorous scientific process based on a very large number of cases.
Screening the moles on your body substantially reduces the chances of succumbing to skin cancer thanks to early diagnosis. If a melanoma grows unchecked into the skin to a depth of 4 mm, this reduces your chances of survival by 20% at five years. The importance of dermoscopy is about specificity, helping doctors to cut out early malignant tumors and not to cut out benign lesions.
Early diagnosis is only possible if you check suspicious moles regularly, at least once a year, or even more frequently if you have a family history of melanoma. Dermoscopy ensures that you will only get a biopsy if necessary. Our facility is one of the few in Ho Chi Minh City that offers this diagnostic opportunity.
 Chúng tôi sử dụng cookies để cải thiện trải nghiệm của người dùng khi truy cập trang web này
Chúng tôi sử dụng cookies để cải thiện trải nghiệm của người dùng khi truy cập trang web này